Abstract
Background: Young adults (22-39y) with ALL treated at an NCI-designated Comprehensive Cancer Center (CCC) have a superior survival when compared with those treated at a non-CCC site. (Wolfson et al, CEBP, 2017) Despite superior outcomes, specialized cancer centers (such as CCC) have been generally criticized for a higher cost of cancer care (Nardi et al, JNCCN, 2016). However, the magnitude of difference in cost of care for ALL patients by treatment site has not been explored. Here we examine cost of cancer care at CCC and non-CCC sites in YA with ALL.
Methods: Using commercial insurance data (OptumLabs® Data Warehouse), we established a cohort of 309 patients with ALL diagnosed between 2001 and 2014, at age 22y to 39y. Patients were included if they had ≥30 days of continuous insurance enrollment after ALL diagnosis, were treated with chemotherapy, and were followed from diagnosis until 3y, disenrollment, or 3/31/2017, whichever came first. Patients undergoing hematopoietic cell transplant were not included in the current analyses. Primary outcomes included total monthly medical costs paid by: (1) health plan; (2) patient (out-of-pocket [OOP] costs). The primary predictor of interest was the classification of the facility where the patient received cancer-related treatment, as NCI-designated CCC vs. non-CCC. Multivariable models were adjusted for age, sex, race/ethnicity, income, education, comorbidity, year of diagnosis and radiation therapy. Monthly costs were modeled using generalized linear models with log link (gamma distribution); bootstrapping obtained 95% confidence intervals (CI). To accommodate censoring, each one-month cost was weighted by the inverse probability of not being censored. Adjusting for covariates, average costs were estimated by CCC status at each monthly interval. Monthly costs were summed over the 36-month study period, and adjusted at the claim-line level to reflect 2016 pricing.
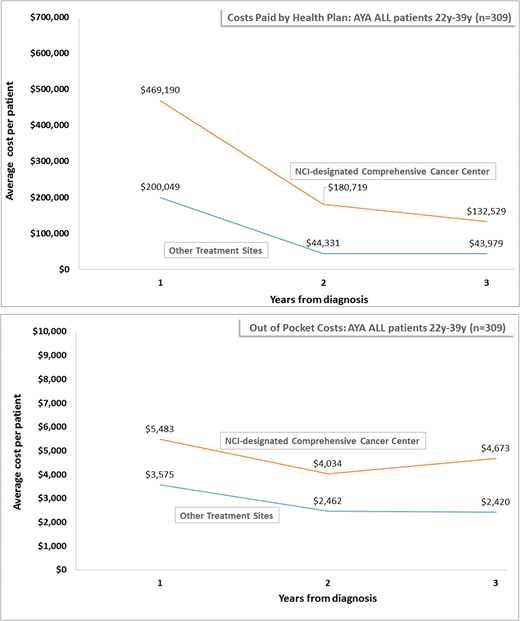
Results: Patients were diagnosed at a median age of 32y (range 22-39); 53% of the cohort was male, 46% non-Hispanic white, 42% had some college education or higher, and 70% had an annual household income of ≥$50,000. Following diagnosis, patients were enrolled in the insurance plan for a median 753 days after ALL diagnosis (34 to 4,899 days). Half of the cohort (n=153, 49.5%) was not treated at a CCC. There was no difference between CCC and non-CCC patients with respect to age, gender, race/ethnicity, education, income, comorbidities, year of diagnosis, or length of follow-up. A greater proportion of patients received radiation at CCC vs. non-CCC (23% vs 13% p=0.02). Costs Paid byHealth Plan: The average unadjusted mean 3y costs paid by the health plan per person (HPP) were $540,822/patient for CCC patients vs. $210,075/patient for non-CCC patients (p<0.001). The average adjusted mean 3y HPP costs were almost 3 times higher for patients treated in CCC vs. non-CCC patients ($782,438/patient vs. $288,359/patient; p<0.001). HPP costs were highest for all patients within the first 12 months (CCC: $469,190/patient; non-CCC: $200,049/patient; p<0.001 [Fig 1]), consistent with the fact that ALL treatment regimens include a more intense first 12 months followed by a longer maintenance phase that relies mostly on oral chemotherapy. OOP CostsPaid by Patient: Unadjusted average 3y mean OOP costs per patient were $9,869 in CCC patients and $5,976 in non-CCC patients (p<0.001). The average adjusted mean OOP costs per patient were 1.7 times higher in CCC as compared to non-CCC patients ($14,190 vs. $8,457; p<0.001). OOP costs were also highest in the first 12 months (CCC: $5,483/patient; non-CCC: $3,575/patient [Fig 2]).
Conclusions: Using a commercial insurance database, we find that for patients diagnosed with ALL between the ages of 22y and 39y, the costs paid by the health plan are 3 times higher for those receiving care at an NCI-designated CCC as compared to a non-CCC site. Along the same lines, out of pocket costs are 1.7 times higher for those receiving care at an NCI-designated CCC as compared to a non-CCC site. The difference in cost is highest during the first year of therapy. We are currently examining the details of what drives the higher cost of care at CCC.
Lyman:Generex Biotechnology: Membership on an entity's Board of Directors or advisory committees; Amgen: Other: Research support; Halozyme; G1 Therapeutics; Coherus Biosciences: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal